Carotid Artery Imaging (CIMT)
Dr. Steve Parcell is the local expert on preventive cardiology, alternatives to statin drugs and similar concerns. Many people today are concerned about the potential side effects of statin drugs and high blood pressure medications.
Were you given a prescription for a medication to control cholesterol by your doctor but are not sure if you should take it? Do you question whether you even have plaque in your arteries? Now there is an easy way to see if you have plaque.
Carotid artery intima-media thickness (CIMT) measured by ultrasound has been shown to be correlated with the presence of cardiovascular disease and is now accepted and used as a marker for atherosclerotic disease. In the Cardiovascular Health Study, increases in the CIMT of the carotid artery were associated with an increased risk of heart attack and stroke in older adults without a history of cardiovascular disease. Common carotid IMT greater than 0.87 mm and Internal Carotid IMT greater than 0.90 mm were associated with a progressively increased risk of cardiovascular events. For each 0.20 mm increase in CCA IMT, the risk increased by almost 30%. IMTs above 1.18 mm were associated with more than a 2-fold increase in the risk of a cardiovascular event over 6 years.
Also, several studies evaluated the effect of statins on the progression of atherosclerosis using imaging of CIMT as an outcome measure. In these studies carotid IMT was used a surrogate marker for coronary atherosclerosis. The LIPID trial randomized 522 subjects to receive pravastatin 40 mg/day or placebo in addition to a low-fat diet. Total cholesterol, triglycerides, HDL, and LDL cholesterol were measured at randomization repeatedly during follow-up. Ultrasound scans of the common carotid artery were performed before randomization, and after 2 and 4 years using B-mode ultrasonography. The study showed a regression of the common carotid artery IMT following pravastatin therapy.
According to recent evidence from the ARBITER 6-HALTS trial, treatment with extended-release niacin, in combination with statin therapy, significantly increases HDL-cholesterol levels and causes a small, but significant, reduction in carotid intima-media thickness. Niacin alone also reduces CIMT.
Ten patients were supplemented with pomegranate for one year and five of them continued for up to three years. Blood samples were collected before treatment and during PJ consumption. In the control group that did not consume pomegranate, CIMT increased by 9% during 1 year, whereas, pomegranate consumption resulted in a significant IMT reduction, by up to 30%, after 1 year.
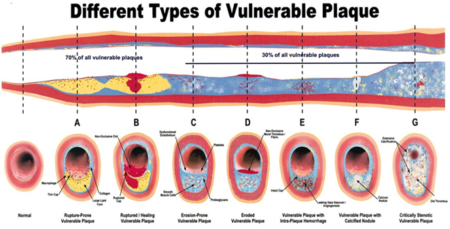
Increased intimal–medial thickness (CIMT, IMT) of the common carotid artery as assessed by ultrasound is an index of atherosclerosis, and is associated with symptomatic coronary artery disease. In addition, IMT is also predictive of cerebrovascular disease, stroke, left ventricular hypertrophy, and coronary artery calcium, ankle brachial index kidney disease. It is widely accepted that IMT is the only surrogate end point for CAD that is endorsed by clinical studies. This is evidenced by the fact that the US Food and Drug Administration recognize IMT as a valid end point in the evaluation of new drugs. It can also identify the most dangerous type of plaque: vulnerable plaque.
The CIMT determines early atherosclerosis in the carotid artery by measuring the diameter of the media and intima, which is where foam cells accumulate in the early stages of atherosclerosis. In healthy adults CIMT ranges from 0.25-1.5 mm. Normal values based on age and gender for black-and-white races have been established. This test is especially useful for asymptomatic patients between ages between 40 and 70 years old.
CIMT is different from the standard Carotid Doppler Ultrasound which measures blood flow velocity. Faster velocity indicates stenosis by virtue of a narrowing of the artery. Unfortunately, in the early stages of plaque formation, there is little narrowing. Thus, a standard carotid Doppler will not identify subtle thickening of the arterial wall and may miss subclinical atherosclerosis and the opportunity to begin treatment early, potentially mitigating the need for a surgical procedure down the road.
Since the 1990s, many statin drug trials have used CIMT for evaluating the regression and progression of atherosclerosis . CIMT has been shown in large-scale, prospective studies (Atherosclerosis Risk in Communities Study, Multiethnic Study of Atherosclerosis ) to be an independent predictor of heart attack and stroke. CIMT is more accurate in predicting heart attack and stroke than any other risk factor alone and increased CIMT is an independent risk factor even in the absence of any other risk factors. Call to schedule!
OTHER RESOURCES
2010 ACCF/AHA Guideline for Assessment of Cardiovascular Risk in Asymptomatic Adults
Imaging Guidelines for Screening CV Risk
Society for Heart Attack Prevention and Eradication
Society of Atherosclerosis Imaging and Prevention
The ARIC Study – CIMT and Presence or Absence of Plaque Improves Prediction of CHD Risk
CAC and CIMT in the Multi-Ethnic Study of Atherosclerosis (MESA)
Asymptomatic Atherosclerosis Book
CardioHealth Station by Panasonic (carotid ultrasound)
Carotid IMT received a higher level of recommendation in the 2010 ACCF/AHA Guidelines than many other widely used tests such as:
● Advanced Lipoprotein Analysis, including Lp(a)
● C-Reactive Protein
● Hemoglobin A1C
● Lipoprotein-associated phospholipase A2 (Lp-PLA2)
● Resting ECG (in those without HTN or DM)
● Resting Echocardiography
● Genotype Testing
● Exercise ECG
● Stress Echocardiography
