Eosinophilic Esophagitis: A Once Rare Condition on the Rise
Eosinphilic esophagitis (EoE) has historically been known as a rare allergic condition. However, it is becoming increasingly more common and can occur at any age, from infants to adults. It can manifest with mild symptoms such as occasional difficulty swallowing, throat pain, vomiting, and more serious incidents of food impaction in the esophagus. In this post we’ll discuss the symptoms of EoE, how it’s diagnosed, and the effectiveness of different treatment options including natural options.
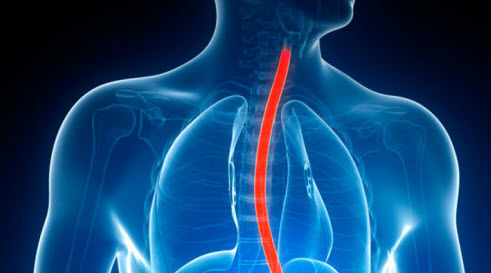
What is Eosinphilic Esophagitis?
Eosinophilic esophagitis is a chronic allergy condition characterized by symptoms of esophageal reflux, nausea, stomach pain, and sometimes vomiting. It is diagnosed when an excessive amount of eosinophils are found in esophageal tissue. In recent years, EoE has emerged as a common cause of upper gastrointestinal (GI) tract problems in both children and adults.
What are Eosinophils?
Eosinophils are white blood cells that are made in the bone marrow and circulate through blood vessels for 8-12 hours. After circulating, eosinophils migrate into a tissue, where they remain for 1-2 weeks.
The Role of Eosinophils
Eosinophil contain around 200 large granules of enzymes and proteins, which break open and release their toxic contents when the eosinophil is activated. Their function is to move to inflamed areas, trap offending substances, and kill cells. They help fight bacteria and parasitic infections and are involved in allergic reactions and inflammatory responses.
Signs and Symptoms of EoE
Infants and toddlers with EoE typically present with feeding difficulties. The symptoms may be similar to gastro-esophageal reflux but the patient will not respond to the same medications.
Nausea, vomiting, and abdominal pain are symptoms more common in school-age children. As the condition continues, dysphagia, chest pain, and difficulty passing solid food can present in adolescents and adults. Chronic inflammation of the esophagus leads to tissue changes and narrowing. Between 33-54% of adults develop a food impaction that necessitates mechanical removal. Patients often adapt feeding behaviors to avoid symptoms, so histories must be carefully taken to discover past symptoms. Children may self-limit food because of pain, so their growth must be monitored.
Eosinophilic esophagitis is strongly associated with other allergic conditions, such as food allergies, allergic rhinitis, asthma, eczema, and environmental allergies. There is usually a family history of allergic disorders. There is a male-to-female prevalence of 3:1 and a high familial inheritance rate, which may be due to a genetic disorder. It is most commonly diagnosed in children younger than three years, but can be found at any age. In one study, the median time between onset of symptoms and diagnosis was 24 months.
Diagnosing EoE
Diagnosis is made through an endoscopy procedure. Endoscopy findings that may indicate EoE include esophageal rings, strictures, white exudates, longitudinal furrows, edema, friability, and esophageal narrowing. These findings alone are not diagnostic of EoE because they may be found with other disorders. In addition to increased numbers of eosinophils, increased numbers of mast cells are often found upon biopsy.
Treatment Options for EoE
Dietary therapy holds significant promise for treating EoE. It may also reverse esophageal fibrosis. Dietary therapy options include:
- Dietary restriction based on likely allergens
- Dietary restriction based on test results
- The use of an elemental amino acid–based formula
The amino acid–based formula has had the most promising results.
One study compared the effectiveness of a six-food elimination diet vs. the standard elemental formula diet. Many consider an elimination diet preferable to the elemental formula because of the ability of a child to still consume food and because of the poor taste of the elemental formula. Of 60 children studied, 35 children were treated with a diet that excluded cow’s milk protein, soy, wheat, egg, peanut, and seafood. The other 25 children consumed only a crystalline amino acid–based elemental formula. After six weeks, 74% of the elimination diet group and 88% of the elemental formula diet group had significant improvement with less than ten eosinophils per high-power field on histological examination.
Another study compared the effectiveness of an elimination diet, elemental diet, and swallowed fluticasone propionate in 17 patients. The findings were as follows:
- Fifteen participants had allergy symptoms and gastrointestinal symptoms, including rhinoconjunctivitis, atopic dermatitis, asthma, aeroallergen allergy, and IgE food allergy
- The food allergens found were cow’s milk, eggs, wheat, fish, and nuts
- Two out of two participants on the elemental diet responded
- Five out of 12 participants on the elimination diet responded
- One out of three on the swallowed corticosteroids responded
- Of the non-responders to the elimination diet, one responded to the elemental diet, and one responded to the fluticasone
- The participants on the elemental diet responded well on sequential reintroduction of foods so that offending foods could be identified and avoided
Simple IgE testing cannot diagnose all the offending foods because the allergen response to food implicated in EoE is not solely IgE mediated. Any food can be a culprit, which may necessitate a strict elemental formula diet for one to three months. Milk, eggs, nuts, beef, wheat, fish, shellfish, corn, and soy are among the most common offending foods.
How Seasonal Variation Affects EoE
Airborne allergens are being found to play a role in EoE. In a review of 314 cases, a significant increase in food impaction was found during the summer and fall, especially if the patients also had atopic disorders. The authors associated this with the presence of dust mites. Another study showed that an increase in the diagnosis of EoE correlated with grass pollen counts in Washington State.
Avoidance and treatment of aeroallergen exposure, as well as food allergens, may be a necessary step for some individuals with EoE.
The Effectiveness of Drug Therapy
- Corticosteroids have been shown to improve symptoms, but the effect does not last when the corticosteroids are stopped. Long-term use of corticosteroids is not recommended because of their adverse effect, especially in children.
- Budesonide is safe and effective for short-term use. It may reverse esophageal fibrosis but has the potential adverse effect of fungal infection.
- Montelukast sodium has been shown clinically to manage symptoms of EoE and may be a better choice than corticosteroids relative to adverse effects
- Fluticasone has been demonstrated to be effective in some cases of EoE
Natural Treatments for EoE
Natural treatment shines as a path forward to healing from EoE. As mentioned earlier, an elimination diet is the best approach to finding foods that are the underlying cause of EoE. Food allergy testing that includes IgG, IgE, and other inflammatory markers may provide a way to identify offending foods when an elimination diet is too difficult to follow.
Supplements
One or more of the following supplements have been found to alleviate symptoms and heal inflamed tissue as offending foods are eliminated:
- Manuka Honey: one study found it able to repair wounds and inflamed tissue
- Deglycyrrhizinated licorice (DGL), slippery elm and aloe vera gel: can reduce acid reflux and coats and heals esophagus tissue
- Ginger and Magnesium: may play a role in increasing the tone of the lower esophageal sphincter to reduce esophageal reflux
- Curcumin: may reduce inflammation associated with EoE
- Melatonin: A study published in 2010 showed that melatoninhas mucosal protective effect with inhibiting gastric acid secretion, while increasing gastrin release, which stimulates the contractility of lower esophageal sphincter reducing gastro-esophageal reflux.
Mast Cell Stabilizers
Mast cells release inflammatory mediators, and several human and animal EoE studies suggest that mast cells might contribute independently or in tandem with eosinophils to esophageal inflammation. The mast cell mediator prostaglandin D2 was found in one study to induce eosinophil activity in an EoE in guinea pigs. Another study found that IgE-bearing mast cells are increased in the esophageal mucosa and smooth muscle layer of EoE patients. There is a double-blind, randomized controlled study examining the safety and efficacy of cromolyn sodium for the treatment of EoE.
Biofeedback
Another area that has been studied is the effectiveness of adding biofeedback-assisted relaxation training in addition to medication for children with duodenal eosinophilia. Compared with children taking medication alone, children who received medication plus biofeedback training, reported decreased pain intensity, shorter duration of painful episodes, and greater clinical improvement.
Solutions for EoE are Prevalent
Although EoE is on the rise, it’s a condition that responds to one or more simple solutions. We recommend that patients try identifying and avoiding food triggers, undergo treatments to heal inflamed tissue and strengthen the tone of the lower esophageal sphincter, try calming mast cell activation, and/or biofeedback therapy.
Are you suffering from EoE? Contact us to discuss your options: 303-884-7557.

