EDTA Chelation Therapy: A Promising Ally in the Fight Against Atherosclerosis

In the modern medical era, atherosclerosis—the buildup of plaque within arterial walls—remains a leading cause of cardiovascular morbidity and mortality. While standard treatments, such as statins, antihypertensives, and lifestyle modifications, have significantly improved outcomes, they do not reverse existing plaque or address certain environmental factors that contribute to vascular disease. Emerging research suggests that EDTA chelation therapy, long relegated to the periphery of cardiovascular medicine, may offer untapped potential, particularly for patients with diabetes and established coronary artery disease.
What Is EDTA Chelation Therapy?
Chelation therapy involves the intravenous administration of ethylenediaminetetraacetic acid (EDTA), a synthetic amino acid that binds to heavy metals and minerals in the bloodstream. Once bound, these complexes are excreted through the urine. Originally developed to treat lead poisoning, EDTA has gained interest in cardiology due to its unique vascular effects.
How Chelation May Work Against Atherosclerosis
EDTA chelation offers several biologically plausible mechanisms by which it may reduce atherosclerotic burden and prevent cardiovascular events:
- Reduction in Heavy Metal Load
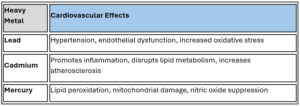
Toxic metals such as lead, mercury and cadmium are independently associated with increased cardiovascular risk. EDTA has a high affinity for these metals, and studies have demonstrated a significant reduction in body burden after therapy. Removing these toxins reduces oxidative stress, a known contributor to endothelial dysfunction and plaque instability. - Decreased Vascular Calcification
EDTA also binds calcium, potentially softening calcified plaques and improving arterial compliance. While the exact impact on plaque regression is under investigation, this decalcification effect may improve perfusion and reduce ischemic risk. - Improved Endothelial Function
Chelation reduces oxidative stress and inflammation, leading to improved nitric oxide bioavailability. This helps restore endothelial integrity, a critical barrier against atherogenesis. - Enhanced Circulation
Patients often report symptomatic improvements in peripheral vascular disease, likely due to better microvascular flow and decreased blood viscosity—both of which support cardiovascular health.
The Evidence: What the TACT Trial Revealed
The Trial to Assess Chelation Therapy (TACT), sponsored by the National Institutes of Health, was the first large, randomized, placebo-controlled study to evaluate EDTA’s effect on cardiovascular outcomes. Conducted on 1708 post-myocardial infarction patients, TACT showed:
- A modest but significant reduction in the composite endpoint (death, MI, stroke, revascularization, or hospitalization for angina).
- A 41% relative risk reduction in this endpoint among diabetic patients.
- A 43% reduction in all-cause mortality in diabetic patients receiving EDTA.
These results were particularly notable because they occurred despite patients being on guideline-directed medical therapy.
The ongoing TACT2 trial, specifically focused on diabetic patients with coronary disease, aims to validate and expand on these findings. Preliminary signals continue to support the cardiovascular benefits of EDTA chelation in this high-risk group.
EDTA Chelation: A Complement, not a Replacement
EDTA chelation is not a substitute for proven therapies like statins, ACE inhibitors, or revascularization when indicated. However, for patients who have experienced recurrent events despite optimal medical therapy, exhibit elevated heavy metal levels, or have diabetes and a high burden of vascular calcification, chelation may serve as a valuable adjunct to standard care.
Safety and Administration
Modern EDTA protocols—such as those used in TACT—are administered in a controlled setting over 30+ infusions and have demonstrated a strong safety profile. Adverse effects are rare and usually mild, especially when calcium EDTA or disodium EDTA is dosed correctly and renal function is monitored.
Conclusion: An Underutilized Therapeutic Avenue
EDTA chelation therapy challenges conventional approaches to cardiovascular prevention by addressing underlying environmental and inflammatory contributors to vascular disease. While further studies are warranted, especially imaging-based trials to assess plaque dynamics, the existing evidence—particularly in diabetic patients—is compelling.
As medicine evolves toward personalized and integrative care, EDTA chelation deserves renewed attention—not as a fringe therapy, but as a promising adjunct in our fight against one of humanity’s deadliest conditions.
Contact NatureMed to make an appointment with Dr. Steve Parcell 303-884-7557
References:
Lamas GA, Goertz C, Boineau R, Mark DB, Rozema T, Nahin RL, et al.
Effect of disodium EDTA chelation regimen on cardiovascular events in patients with previous myocardial infarction: The TACT randomized trial.
JAMA. 2013 Mar 27;309(12):1241–1250.
PubMed Link:
https://pubmed.ncbi.nlm.nih.gov/23532240/
TACT2 – Ongoing Trial (As of 2025)
Trial Registry:
Title: Trial to Assess Chelation Therapy 2 (TACT2)
ClinicalTrials.gov Identifier: NCT02733185
Sponsor: Mount Sinai Medical Center of Florida
Principal Investigator: Gervasio A. Lamas, MD
Status (as of 2025): Ongoing, not yet published results.
Navas-Acien et al., 2007 – JAMA (Landmark Study)
Title: Lead, cadmium, smoking, and increased risk of peripheral arterial disease
Authors: Ana Navas-Acien, Eliseo Guallar, et al.
Journal: JAMA. 2004 Jun 25;289(18):2271–2279.
DOI: 10.1001/jama.289.18.2271
Key Findings:
- Data from NHANES showed that elevated blood levels of lead and cadmium were independently associated with higher risk of peripheral arterial disease (PAD).
- This remained significant even after adjusting for smoking and other cardiovascular risk factors.
Link: PubMed
Tellez-Plaza et al., 2013 – Circulation: Cardiovascular Quality and Outcomes
Title: Cadmium Exposure and All-Cause and Cardiovascular Mortality in the U.S. General Population
Authors: Maria Tellez-Plaza, Eliseo Guallar, et al.
Journal: Circ Cardiovasc Qual Outcomes. 2013 Nov;6(6):651–658.
DOI: 10.1161/CIRCOUTCOMES.113.000208
Key Findings:
- Cadmium exposure (measured in urine) was associated with increased all-cause and cardiovascular mortality, especially in individuals with hypertension.
Link: PubMed
Houston MC, 2011 – Journal of Clinical Hypertension (Review)
Title: Role of Mercury Toxicity in Hypertension, Cardiovascular Disease, and Stroke
Author: Mark C. Houston, MD
Journal: J Clin Hypertens. 2011 Dec;13(8):621–627.
DOI: 10.1111/j.1751-7176.2011.00543.x
Summary:
- Mercury exposure was linked to oxidative stress, endothelial dysfunction, increased inflammation, and hypertension, all of which contribute to atherosclerosis.
- The review outlines the mechanistic pathways by which mercury exacerbates cardiovascular risk.
Genchi et al., 2017 – Environmental Toxicology and Pharmacology (Comprehensive Review)
Title: Mercury exposure and heart diseases
Authors: Giuseppe Genchi et al.
Journal: Environ Toxicol Pharmacol. 2017 Feb;50:1–7.
DOI: 10.1016/j.etap.2017.01.006
Highlights:
- Reviews both experimental and epidemiological evidence showing that mercury promotes lipid peroxidation, impairs mitochondrial function, and fosters vascular inflammation.